It’s easy to lose your perspective in the rush of surgery. As a children’s heart surgeon, it has been my life’s greatest privilege to be part of many wonderful moments that changed lives for thousands of patients in Toronto, Louisville, Dallas, New Orleans, and now, in Richmond.
Recently, a patient gave me pause to step back, savor the moment, and celebrate the wealth of talent here in Richmond that can be brought to bear when a child needs it.
This is the story of Kai’Ayshia, a beautiful 4-year old girl, and her mother, whose concern grew with the growing stream of doctors checking on them and the echocardiography screen being used to image her heart.
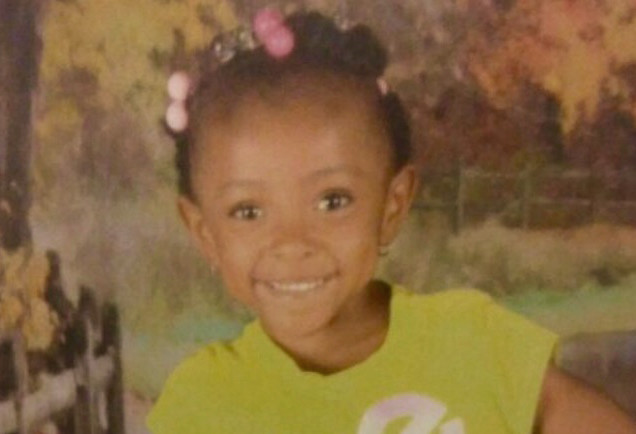
It turns out Kai’Ayshia had developed a massive pulmonary embolus, a blood clot in the major arteries to the lungs, that was putting major strain on her heart that would surely kill her if we couldn’t fix it quickly.
Her oncologist and cardiologist discovered the clot and sounded the alarm at 3 p.m. On my way to the bedside, I asked the children’s heart team to cancel their evening plans and get ready for a long night.
On my way I smiled — that worried smile I get when I catch myself running — because I’ve been told it’s never good when you see a pediatric heart surgeon running through the hospital.
And then I started thinking … wait, why is an oncologist involved?
I soon learned that Kai’Ayshia case was even more complicated than I thought.
For years, she had been battling a large, benign tumor of the chest with a team of pediatric general surgeons, pediatric plastic surgeons, and interventional radiologists. Just weeks before, the tumor had invaded her spinal canal and could have left her paralyzed were it not for the swift action of our neurosurgeons.
She was just starting to walk again. Now, looking at her X-rays, not only was there a huge clot in her lungs threatening to stop her heart, there was also a large tumor between me and Kai’Ayshia heart. That upped the ante for both of us.

Everyone literally dropped what they were doing and came to help. In concert, we decided that the tumor increased the risk for conventional surgery that I had planned, but we also decided that Kai’Ayshia’s heart was too fragile to manage in radiology with no safety net. So we took her to radiology with a new script.
Normally, we anesthetize children before we put in safety monitoring lines. Kai’Ayshia was too unstable for this, so our pediatric cardiac anesthesiologist snuck those lines into a frightened 4-year-old by distracting her with an empathic resident who played the movie Frozen on a cell phone and sang the songs with Kai’Ayshia. I was impressed.
With my partner and cardiac OR team scrubbed and ready, Kai’Ayshia was put under anesthesia and, without wasting a second, immediately placed on ECMO (Extracorporeal Membrane Oxygenation) through large tubes in her neck. ECMO is, in essence, a heart-lung machine that would protect her brain and other vital organs if her fragile heart arrested.
With that safety net deployed, our cardiologists placed a probe in her esophagus to image the pulmonary arteries and help guide the interventional radiologists. The radiologists placed tubes through the veins in her leg, threaded them through the right side of her heart and into her lungs, where they were used to suction out the offending clots.
At the end of several hours, the radiologists declared it “their most successful suction embolectomy ever.”
After I had put Kai’Ayshia on ECMO, I stepped back into a support role and began assessing the team in action. There was such a willingness, an excitement, in a huge team of diverse adult and pediatric specialists, to lock arms in a protective shell of expertise around a child who might never know how we could have lost her that day.
It was a high-wire, high-tech plan, executed like we had been working together for years. Our radiologist must have felt the same the next day when he noted that it was “truly medicine at its finest.” That spirit, that eagerness to take on things that seem insurmountable, is the essence of the Children’s Hospital Foundation Heart Center, Children’s Hospital of Richmond at VCU, and VCU Health.
It was expertise, ingenuity, and caring. And, for the family, it was hope. I write so you might see the team as I could in that moment, proud of them to be sure, privileged to be a part of it, but thankful that this kind of expertise is here in Richmond for all kids like Kai’Ayshia.
The end of the story?
For Kai’Ayshia, the team walked her back to the ICU after midnight, enjoying the relief and the back-slapping comradery that comes at the end of a treacherous day that, ultimately, just went great. The team tucked her into the safety of the pediatric ICU and disbanded. By the next morning her heart had recovered.
In the PICU, we took her off ECMO, removed the tubes in her neck and took her off the ventilator. Soon, Kai’Ayshia was sitting in bed and whispering her biggest worry in her devoted mother’s ear,
“Can I have ice cream for breakfast?”
She did.

