Diabetes education
Helping children manage diabetes with our comprehensive education program
Our diabetes team is here to help guide you as you become comfortable learning more about your child's diabetes condition and care needs. We offer educational materials that will help you through the learning process of day-to-day diabetes management at home.
Diabetes education is an important component of successful, healthy diabetes management
We're proud to be an American Diabetes Association recognized program with certified educators and to help patients and families navigate their journeys with type 1 and 2 diabetes. These services include education about taking your medicines, how to monitor blood sugar levels, healthy eating, treating high and low readings, preventing complications and coping with diabetes.
Diabetes education services are billed through insurance.
Our diabetes education program helps patients and families with the following
- Understanding diabetes
- Managing diabetes care
- How to safely administer medications
- Monitoring blood sugars and how to treat highs and lows
- What to do when your child is sick
- How to safely stay active
- Assisting with diabetes management at school
- Planning your child's meals and snacks
- Ongoing education on the latest in diabetes technology resources and more
Download our comprehensive diabetes handbook
What is diabetes?
Diabetes is a condition that affects how your body turns food into energy. If you have diabetes your body either doesn't make enough insulin (which acts like a key to let the blood sugar into your body to use as energy) or can't use the insulin it makes as it should. Because of this, the level of sugar in your blood remains higher than normal, which can cause several health problems.
What are the differences between type 1 and type 2?
The two types of diabetes are type 1 and type 2. Both make blood sugar levels higher than normal but in different ways.
Type 1 diabetes: If you are diagnosed with type 1, also called juvenile diabetes, your pancreas does not make insulin. If you have type 1 diabetes, you will depend on daily treatments through insulin injections or an insulin pump to control blood glucose levels.
Type 2 diabetes: With type 2 diabetes, your body either resists the effects of insulin or does not produce enough insulin. While historically, type 2 diabetes has been referred to as adult-onset diabetes, more children are being diagnosed with type 2 diabetes and require diabetes management plans to help lose weight, eat well and exercise. If diet and exercise aren't enough to manage your blood sugar well, you may also need diabetes medications or insulin therapy.
For our families where it is uncertain if the diagnosis is type 1 or type 2 diabetes, we explain that the labs obtained while in the hospital will help to confirm a diagnosis, but explain that the only treatment at the time of hospitalization is the use of insulin.
Symptoms of diabetes:
The symptoms of type 1 or type 2 diabetes may include:
- Urinating (pee) a lot, often at night
- Being very thirsty
- Losing weight without trying
- Feeling very hungry
- Feeling very tired
Managing diabetes care
Appointments
After the initial diagnosis, your child should be seen within one to two weeks, at one month and then at least every three months as needed for follow-up. Your initial follow-up appointments with your child's provider will be scheduled prior to discharge from the hospital.
Follow up appointments are generally scheduled three months in advance. Please make future appointments as you are leaving your present appointment.
What to bring to appointments?
- Glucose meter
- 2 week+ of glucose log
- List of current medications
- List of questions
- 3-day food log
 Prescription refills
Prescription refills
Request your prescription refills through the patient portal or by calling (804) 828-CHOR (2467) and follow the prompts for prescription refills. If you are leaving a message, be sure to include your pharmacy's name, address and phone number and the medication and dosage.
Please allow three business days for refills. This allows us time to review your chart, which is necessary to ensure accurate refills.
Reporting of blood sugar
For blood sugar between appointments, please send at least 7 days of blood sugar numbers, including insulin doses, via the patient portal (preferred method), fax or email. Logsheets are available in the resources and forms section of the guide.
Prior to an appointment: If your child's technology is downloadable, please plan to do so from home, the day prior to the appointment.
If your child is using diabetes technology and you have completed a download, please advise the team so the data can be reviewed.
Always include your name, your child's name and date of birth, and a daytime phone number where you can be reached.
Medications
Our team of diabetes educators will help you understand how to safely administer your child's medication doses based on your provider's recommendations.
Monitoring blood sugars and how to treat highs and lows
You and your child are coached on how to monitor blood sugar using a glucose meter. You will go home with one meter and a prescription for a second meter, to ensure one can be left at school (if needed).
You and your child will be coached how to manage high and low glucose readings.
Low blood sugar
Hypoglycemia, or low blood sugar, is defined as a glucose reading less than 70 mg/dL (or less than 80 mg/dL, if your child is younger than 6 years old).
Signs and symptoms of low blood sugar
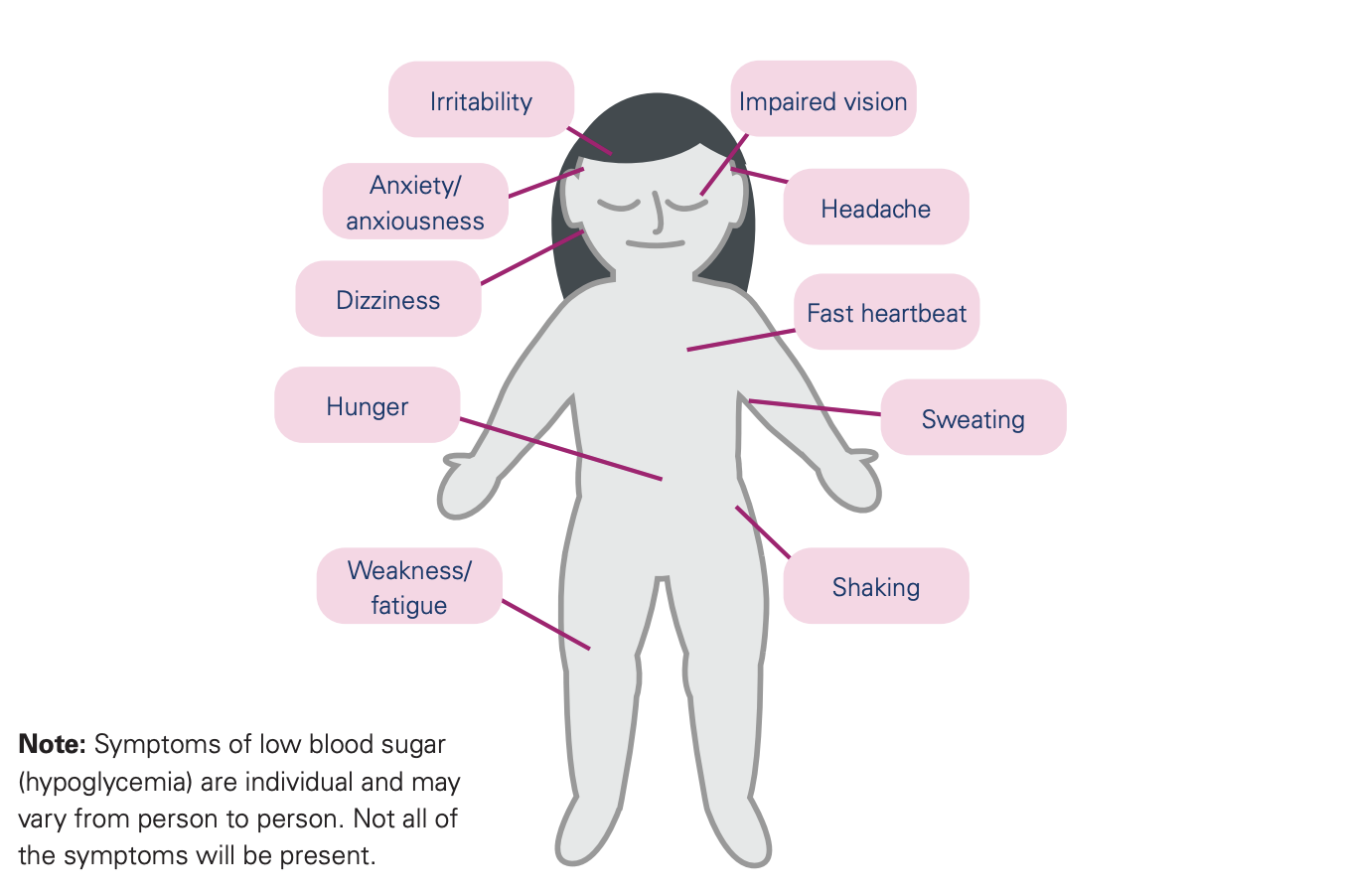 The onset of low blood sugar can occur quickly and the symptoms may vary from child to child.
The onset of low blood sugar can occur quickly and the symptoms may vary from child to child.
- Irritability
- Impaired vision
- Anxiety/anxiousness
- Dizziness
- Headache
- Fast heartbeat
- Sweating
- Hunger
- Weakness/fatigue
- Shaking
High blood sugar
Hyperglycemia is defined as a glucose reading greater than 350 mg/dL.
Signs and symptoms of high blood sugar
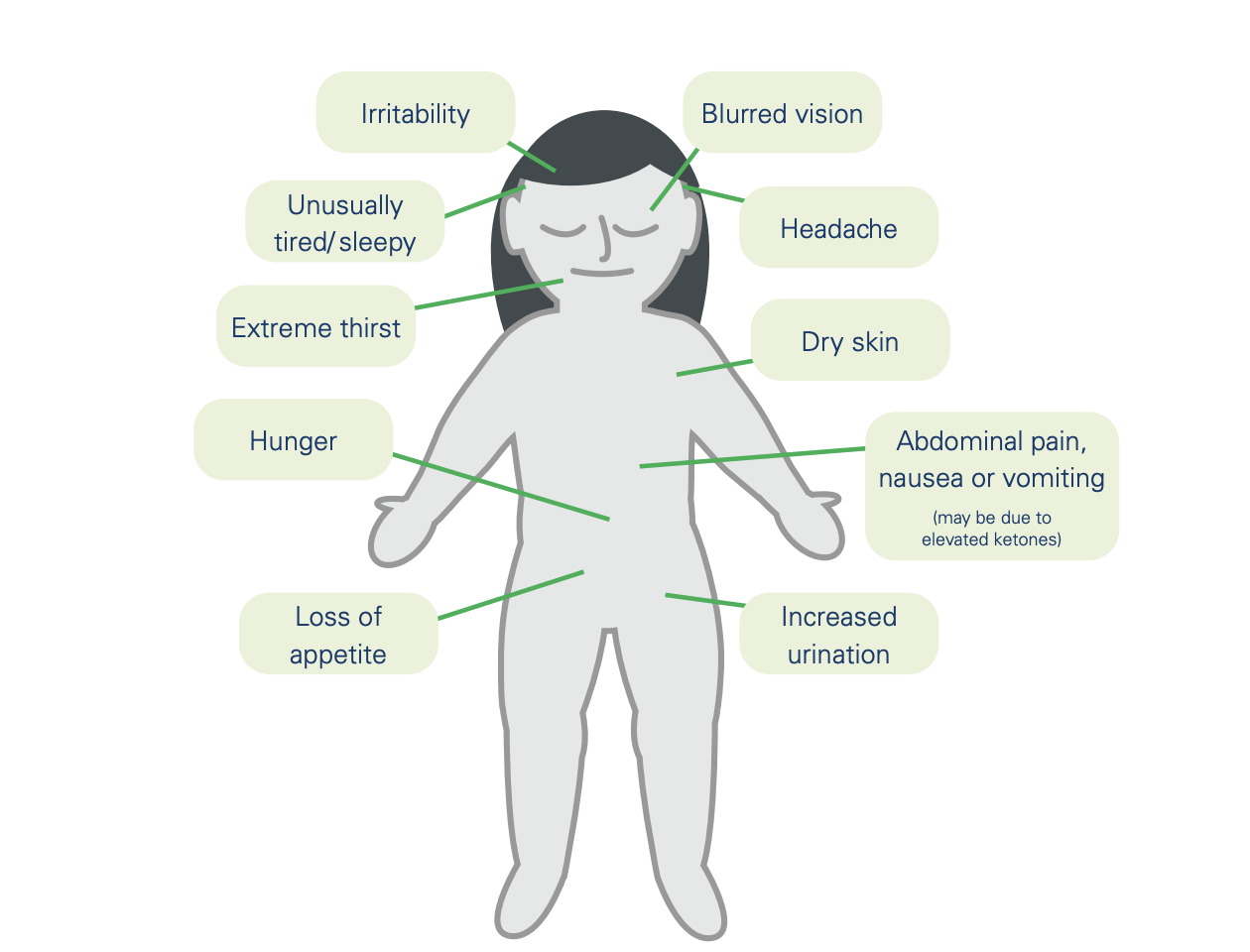 High blood sugar can occur when an individual does not have enough insulin.
High blood sugar can occur when an individual does not have enough insulin.
Here are some usual signs of high blood sugar:
- Unusually tired/sleepy
- Dry skin
- Irritability
- Extreme thirst
- Loss of appetite
- Hunger
- Increased urination
- Blurred vision
- Headache
Diabetic Ketoacidosis (DKA)
Signs and symptoms of DKA:
- Unusually tired/sleepy
- Dry skin
- Irritability
- Extreme thirst
- Loss of appetite
- Hunger
- Increased urination
- Blurred vision
- Headache
- Abdominal pain, nausea, vomiting
How to provide treatment for high blood sugar:
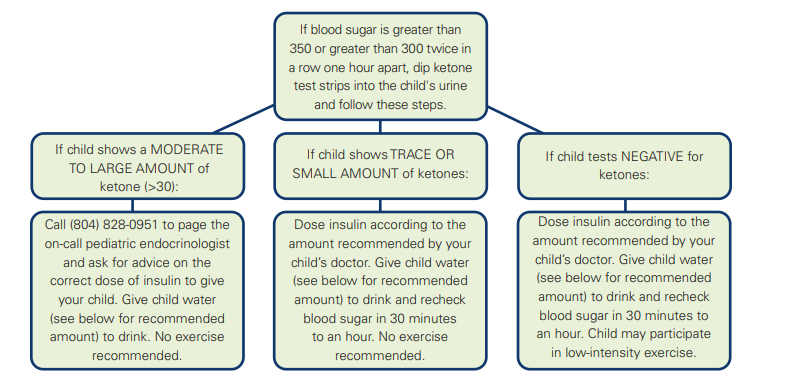
If blood sugar is greater than 350 or greater than 300 twice in a row one hour apart, dip ketone test strips into the child's urine and follow these steps.
- If a child shows a MODERATE TO LARGE AMOUNT of ketone (>30): Call (804) 828-0951 to page the on-call pediatric endocrinologist and ask for advice on the correct dose of insulin to give your child. Give child water (see below for recommended amount) to drink. No exercise recommended.
- If a child shows TRACE OR SMALL AMOUNT of ketones: Dose insulin according to the amount recommended by your child's doctor. Give child water (see below for recommended amount) to drink and recheck blood sugar in 30 minutes to an hour. No exercise recommended.
- If a child tests NEGATIVE for ketones: Dose insulin according to the amount recommended by your child's doctor. Give child water (see below for recommended amount) to drink and recheck blood sugar in 30 minutes to an hour. Your child may participate in low-intensity exercise.
The minimum amount of water recommended is 1 ounce/child's year of age up to 16 ounces. For example:
- 2-year-old child = minimum of 2 ounces of water
- 8-year-old child = minimum of 8 ounces of water
Here are the parameters for blood ketone testing:
- Negative (<1 mmol/L)
- Trace/Small (1-2.9 mmol/L)
- Moderate/Large (>3.0 mmol/L)
Without insulin, diabetic ketoacidosis (DKA) can occur, because the body cannot move sugar from the bloodstream into the cells. Ketones are dangerous and require treatment with appropriate medical therapy (including insulin).
When meeting with our diabetes team, we will review and outline how to properly monitor and treat your child's blood sugars.
What to do if your child is sick
All children experience routine childhood colds or flu. While these illnesses usually aren't serious, they can make diabetes management more challenging.
- Continue your child's long-acting insulin dosing (Lantus, Basaglar, Tresiba, Toujeo, Levemir, NPH/Humulin N)
- Check your child's blood sugar and urine ketones every two to four hours or as instructed by your provider.
- If your child is not nauseated and can eat a regular diet, continue to dose meal-time insulin as advised. Also, encourage them to drink plenty of sugar-free fluids. This will help prevent dehydration and flush ketones out of the body. A minimum of 1 ounce/child's year of age up to 16 ounces each hour of sugar-free beverages is recommended when your child's blood sugar is over 180.
- If your child is not eating well and has blood sugar below 180, give drinks with sugar in them (regular sodas or ice pops, fruit juices, sugared tea, etc.). Contact your provider for meal-time dosing instructions.
- Try to have your child follow regular eating habits. If you are unable to do this, give your child small amounts of sugar-containing foods every hour. A child should eat 15 grams of carbohydrates per hour. Contact your provider for meal-time dosing instructions.
- If there is nausea or vomiting, give only clear liquids (sodas, apple juice or Jell-O). Contact your provider for meal-time dosing instructions.
- Your child may feel more comfortable eating small amounts frequently instead of the customary three meals and snacks.
Call your on-call provider immediately if you notice the following:
- Signs of dehydration, such as:
- Sunken eyes
- Dry, cracked lips
- Dry mouth
- Skin that remains pinched up after being pinched
- Vomiting
- Any change in alertness
- Rapid or shallow breathing
- Blood sugar over 350mg/dL with moderate to large ketones in the urine
- Breath that smells of overly ripe fruit
- Abdominal pain
The phone number to reach us for these urgent concerns is (804) 828-0951 and ask for: “On-call pediatric endocrinologist”
Physical activity
All children with diabetes can participate fully in physical education classes and team sports. To maintain blood glucose levels in target ranges, adjustments may need to be made to insulin and carb intake.
It's also important to check blood glucose levels more frequently during times when your child is active to monitor for low blood sugars.
Important things to know about physical activity and diabetes
- Children should NOT participate in physical activity if they have moderate or high ketones.
- The impact of physical activity on glucose levels can vary.
- The effects of physical activity on blood sugar can last up to 24 hours as sugar stores are put back into the muscles.
- Blood sugars should be checked before, during and after the activity as needed.
- All children should aim for 60 minutes of daily activity for at least five days per week.
Our diabetes educators will help provide suggestions for safely exercising and answer any questions you may have.
Diabetes management at school
Starting your child back to school after they've been diagnosed with diabetes can be stressful. Careful planning and preparation can help ease the transition for all involved.
To make this process as smooth as possible, here's a list of the items needed for school:
- Copy of the Diabetes Medical Management Plan (also called School Form)
- Blood glucose testing equipment and supplies (blood glucose meter, test strips, lancets)
- Ketone strips
- Insulin and insulin delivery system (pens, vials, pen needles, syringes, etc.)
- Pump supplies, if applicable
- Extra batteries for meter, pump, etc., if applicable
- Glucagon Emergency Kit
- Fast-acting carbohydrates (glucose tablets, juice box, regular soda, cake icing gel, etc.)
- Peanut butter, cheese crackers or appropriate snack
How does a school nurse know what to do?
Schools require an updated Diabetes Medical Management Plan (also called School Form) annually before starting a new school year. This form contains up-to-date medication orders and is usually kept by the school nurse.
Most schools will accept this plan on the standard form we provide. You will need to request a new form from us before a new school year.

Planning your child's diet
Our team will help patients plan meals and snacks, provide tips for calculating a child's carbohydrate intake, suggestions for low-carb snacks and more.
