
Positional plagiocephaly is the term doctors use to describe flatness on the back of an infant’s head caused by them lying on it. The incidence of PP has risen from around 2 to 5 percent to as high as 46 percent and is a common complaint that brings families in to see physicians.1,2 Thank goodness this condition does not affect brain growth and can easily correct on its own – or be prevented from even starting – with some simple maneuvering!
Clues and contributing factors
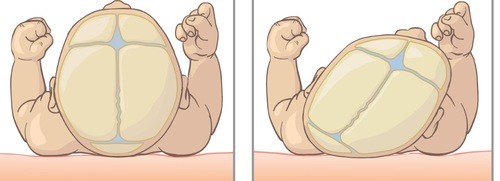
 The most characteristic head shape of a child with PP is that one side of the back of their head is flat, while the forehead and ear on the flat side may be positioned further forward. A head tilt, or “torticollis,” can be observed in 93 percent of children with positional plagiocephaly. This occurs when muscles on one side of the neck are tighter (less able to move than the muscles on other side) which can limit head movement and motion on one side.
The most characteristic head shape of a child with PP is that one side of the back of their head is flat, while the forehead and ear on the flat side may be positioned further forward. A head tilt, or “torticollis,” can be observed in 93 percent of children with positional plagiocephaly. This occurs when muscles on one side of the neck are tighter (less able to move than the muscles on other side) which can limit head movement and motion on one side.
More often than not, PP relates to flatness caused by sleep position. Babies do need to sleep on their back – it’s recommended by the American Academy of Pediatrics for important safety reasons – but if a child lies on their back with their head mainly on one side, a flattened head may result. Factors that may contribute to PP include head preference during sleep, being bottle-fed on the same arm, slower motor development and not enough daily tummy time.
Typical timeline
The timeline for development of plagiocephaly follows the development of the infant. It is usually not present at birth, but over the next six to eight weeks, families or the child’s physician may begin to see flatness. In these first months of life, an infant’s neck muscles are weak and they have a growing, heavy head and a softer skull. It’s not uncommon for some flatness to occur before a child is able to hold their head up on their own.
The flatness may continue to worsen, but usually starts improving between four and six months. This corresponds to an infant getting stronger, being able to roll over, sit up and crawl, and having better control of their upper body. Positional plagiocephaly seldom worsens after the age of four to six months. A majority of kids will improve on their own. In one study, only about 12 percent of children ages 13 to 18 had moderate head-shape differences when measured.2
Repositioning: Start early in life and do throughout the day if needed
The best treatment for positional plagiocephaly is preventing it! To accomplish this, pediatricians suggest early repositioning, or moving the infant so they don’t spend too much time putting pressure on one side of the head when the skull is soft and the brain is growing fast. Infants from birth to 3 months should be placed on their backs, alternating which side their head is turned to, which avoids putting more pressure on one side. Tummy time, which promotes normal shaping of the head and increases neck and upper body strength, should begin in this age group and advance to three sessions of at least 30-minutes a day.
Tummy time is considered to be any activity or position that keeps an infant from lying against a hard surface in one position. It also helps with strengthening neck muscles that help keep the head off one spot. There are great websites that describe various positions and fun exercises to do with an infant that help, including AAP resources Back to Sleep, Tummy to Play and Tummy Time Activities.
If a child already has PP, families should start positioning the child off the flat side the majority of the time. The following are maneuvers that can help prevent or improve PP.
- Alternate the side of the head your baby sleeps or lies on. This is easier to do when the infant is young.
- Move the crib so your baby must turn their head off the flat side to look around the room. Babies will usually begin to recognize windows and bright contrasts as well as where the door is located and tend to look that way. Alternating the wall that the crib is on can help.
- When changing diapers, angle your baby on the side that isn’t flat and change the diaper in that position rather than with child lying flat on their back.
- Place all toys on the opposite side of stroller, swing, crib and infant seat from the flat one to encourage child to look in that direction and turn their head off the flat side.
- Alternate the hip your infant is carried on to encourage them to look both ways.
- When bottle or breastfeeding, position the infant to keep them off the flat side.
- In the car, place a suction toy or mirror opposite the flat side so your baby will want to look that way.
- When your baby is in the swing, bouncy seat, etc., angle the seat in a way that they need to turn their head to the fuller side to watch you or the activities going on around them.
- Providing the recommended amount of supervised tummy time daily is perhaps what’s most important. Again, begin within the first three months and aim for at least three 30-minute sessions each day.
Treating torticollis
If torticollis is present, exercises to loosen the tight neck muscle should be done at each diaper change. These include gently moving child’s head from chin to shoulder and ear to shoulder on each side. Physical therapy may be helpful if the case is severe.
Helmet considerations
If the shape is severe, or has not improved after with repositioning, a helmet that helps mold the shape of the head can be considered.
The AAP suggests at least four to six weeks of repositioning prior to consideration of a helmet. Helmet therapy is not FDA approved in infants less than 4 months of age, and the younger the age of the patient, the faster the head shape will correct. Over 80 percent of head growth occurs in the first year of life, therefore helmets used with children who are over 12-16 months of age are unlikely to produce a noticeable improvement. The average length of treatment is three months. Helmet treatment may be costly and time consuming. Prevention and active repositioning should be the mainstay of treatment in children.
Seeking help
Positional plagiocephaly has become a common finding and occurs when external forces deform the soft skull of infants. We can’t stress enough that the best treatment is prevention and just how important tummy time and alternating “sides” during sleep are in preventing this.
If PP is diagnosed, active repositioning and tummy time will work for most minor or moderate cases. If present, torticollis should be treated by neck strengthening and muscle lengthening exercises. Your pediatrician can recommend physical therapy to help with these exercises. Cranial orthotics or helmets should be postponed until the age of 6 months and used only in severe cases or those that have not improved with repositioning techniques. Thankfully, surgery is not required for positional plagiocephaly.
-Dr. Ann Ritter, pediatric neurosurgeon
1Mawji A, Vollman AR, Hatfield J, McNeil DA, Sauve R. The incidence of positional plagiocephaly: a cohort study. Pediatrics. Aug 2013: 132(2):298-304
2DiRocco F, Ble V, Beuriat PA, Szathamari A, Lohkamp LN, Mottolese C. Prevalence and severity of positional plagiocephaly in children and adolescents. Act Neurochir (Wein). June 16 2019: 161(6): 1095-1098
