
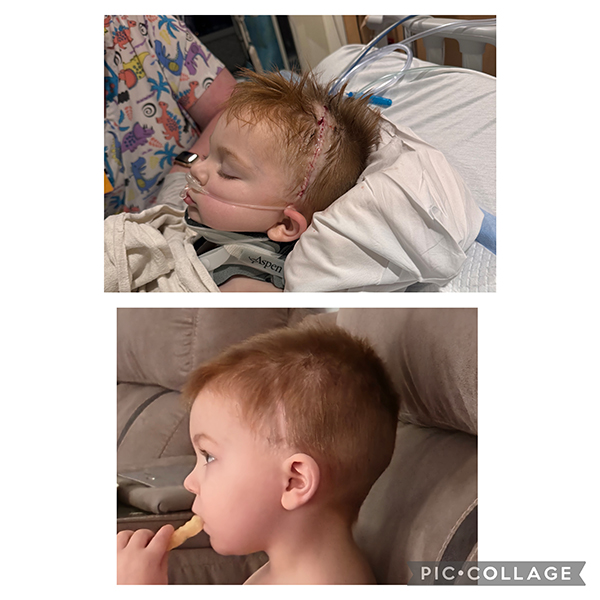
How quick action, and care in the right place, saved Linwood’s life
An evening grocery shopping trip turned into an unexpectedly scary series of events for the Munford family last September. They went to the store around 6 p.m. and, while shopping, 2-year-old Linwood stood up in the basket part of the cart.
“As I went to sit him down so he wouldn't fall out, he jerked his body back away from me, resulting in him falling out of the grocery cart and smacking his head on the floor,” recalled Linwood’s mom, Abby. “He cried for a little bit, but he stopped about 15 minutes later.”
Linny, as his family often calls him, acted normally until about 9 p.m. when his parents were getting him ready for bed.
Choosing CHoR for the right care right away
“We laid him down to change him and then that's when everything took a turn. He was losing consciousness very quickly and we called 911,” added Abby. “They showed up in 7 minutes. Linny was not responsive once the EMTs took him. I remember my dad telling me to get in the car so I didn't see Linny like that.”
Abby’s husband, Chase, told the emergency crew to take their son to whichever hospital they would choose for their own kids. With this direction, and recognizing the severity of Linwood’s injury, they brought him to CHoR, the only Level 1 pediatric trauma center in the region. Meanwhile, Abby and her mom called everyone they knew to ask for prayers as they traveled to the hospital.
What happens in a Level 1 pediatric trauma center
Chase recalled seeing at least 50 medical professionals standing by when the family arrived in the emergency department, each with a job that they did diligently.
“Trauma response is tiered based on the patient’s initial presentation or the report we receive from pre-hospital alerts,” explained Nicole Laurin, RN, pediatric trauma program manager. “For our most severely injured children, which Linwood was, it is a full team response including a pediatric trauma surgeon, pediatric emergency medicine physicians, pediatric anesthesia, pediatric intensivists, pharmacy, respiratory therapy, radiology, an ER medic, and pediatric trauma trained nursing staff from both the ER and pediatric intensive care unit. Additionally a social worker, child life specialist and chaplain also respond to provide additional support to the patient and family. This team response means we are fully ready to provide any lifesaving interventions, quickly evaluate and identify injuries, and move quickly to the operating room or pediatric intensive care unit as needed.”
Linwood was taken straight for a CT scan, which showed a large brain bleed. The team in our emergency department immediately notified our neurosurgery team. Having this and other pediatric subspecialty care available 24/7 is an essential component of a Level 1 pediatric trauma center.
“We took him to the OR as fast as we could move,” said Dr. Jessica Lane, the neurosurgeon who operated on Linwood. “The type of hemorrhage Linwood had can be very dangerous. Because patients with epidural hematomas often have a ‘lucid interval,’ or period of a few hours where they are acting normally after their trauma, families are often falsely reassured that no major injury has taken place. Without surgery, these types of hematomas are often fatal.”
Expert pediatric neurosurgical care at a moment’s notice
 “We had no time to think or plan anything. To save Linwood’s life, the decision was immediate,” added Abby, of the brisk action to get her son into surgery.
“We had no time to think or plan anything. To save Linwood’s life, the decision was immediate,” added Abby, of the brisk action to get her son into surgery.
In the surgery, Dr. Lane opened Linwood’s scalp and removed a portion of skull bone overlying the hemorrhage. She then removed the clotted blood that was exerting pressure on his brain, and identified and cauterized the injured blood vessel to prevent further bleeding. Once all the blood was gone, she reattached his skull bone and stitched him up. He was then transferred to our pediatric intensive care unit for continued monitoring and care.
“We never went a long time without updates. Everyone was so professional, polite and sincere,” said Abby.
Following surgery, Linwood’s prognosis is excellent.
“Linwood looked really good the morning after surgery and we were able to let him go home less than 48 hours after he presented. Seeing him look so great so quickly after surgery – especially knowing how bad the outcome could have been without intervention – is incredibly gratifying,” added Dr. Lane.
After being discharged from the hospital, Linwood came for outpatient appointments with our neurosurgery and physical medicine and rehabilitation (traumatic brain injury) specialists. He has done very well and now only needs to follow up if concerns arise.
A happy Munford family celebrates Linwood’s life and shares a note of caution with other parents
Instead of spending time at doctor’s appointments, Linwood is mastering sight recognition of numbers and letters. He loves food (especially bananas and eggs), monster trucks, excavators, Spiderman, Wawa, his brother, and Mom and Dad – though not necessarily in that order. Linny and his parents also made a trip to Chesterfield Fire Station 15 to thank them for being the first in a chain of professionals who helped save his life.
Linwood is always on the go, but his parents won’t complain.
“It's amazing to watch him learn and grow after his injury. He is bubbly and full of energy. We like to say he doesn't have an off button,” added Abby. “If I could pass any advice to other parents, it would be to ALWAYS buckle your child in. You might think it won't happen to you, but we are proof that anything can happen. After 6 months, it still pulls at my heart, but it makes me appreciate life even more. We thank God every day for Dr. Lane and her team giving Linwood another chance at life. Being that he isn't even 3 yet, he has so much life to live now. He’s our little miracle.”
Seeking medical care after your child hits their head
It can be difficult to know exactly when to seek medical attention when a baby or kid hits their head. If you notice any of the following symptoms immediately or in the 24-48 hours following the injury, take your child to the emergency department right away:
- Blood or clear fluid coming from the nose or ears
- Confused or disoriented state
- Difficulty speaking or walking (in children who have already mastered these skills)
- Excessive drowsiness
- Loss of consciousness (even if brief)
- Seizures
- Severe headache
- Unusual behavior
- Vomiting
